
Often when a general plastic surgeon performs eyelid surgery, they send the patient to an ophthalmologist if they complain of dry eye symptoms. The plastic surgeon essentially puts the burden of the surgical outcome onto the ophthalmologist, who is now put in a difficult position of managing the patient’s dry eyes for years, long after the plastic surgeon compromised eyelid function.
A systematic approach to identifying the degree of dry eye prior to surgery is very important. Further, specific aspects of eyelid anatomy directly affect eyelid function, and could impact future dry eye management.
Lower Eyelid Surgery for People with Dry Eyes
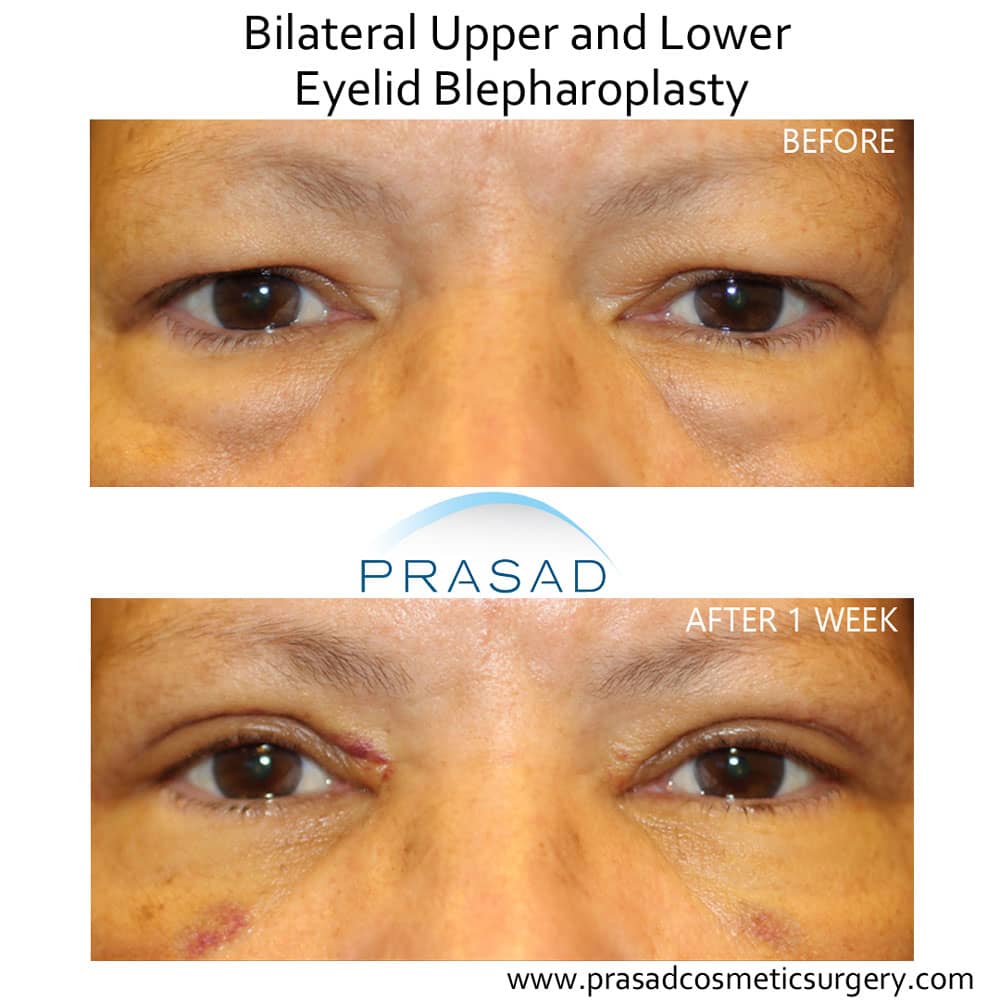
Lower eyelid surgery for eye bag removal is a very popular procedure. The lower eyelid is very important for proper distribution of tears over the eyes. You can think of this interaction of the upper and lower eyelids working like a windshield wiper to evenly distribute tears over the surface of the eyes. If there is any change in the anatomy of the lower eyelid, particularly the position of the eyelid margin, this tear distribution function will be impacted
A very commonly performed technique for lower eyelid surgery is the transcutaneous method, where an incision is made below the eyelashes to remove and sculpt the fat which causes eye bags. It’s common practice to also remove skin at the same time in an attempt to improve fine lines and wrinkles under the eyes. Without managing the critical structural support of the lower eyelid, this technique often compromises the position of the lower eyelid, as well as its function. The result is a pulled down appearance referred to as lower eyelid retraction, which can also cause an inability to fully close the eyes, resulting in eye exposure and dryness.
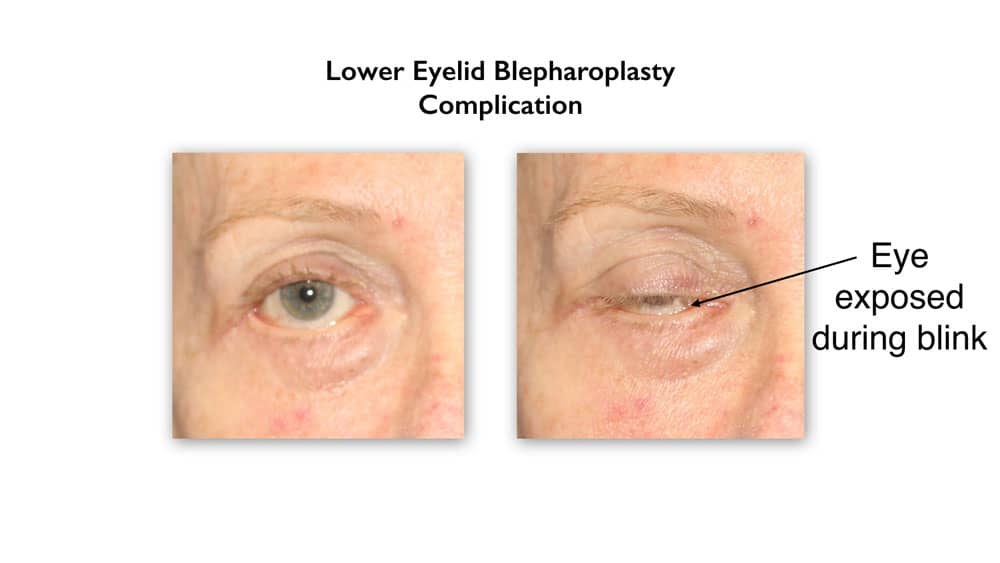
Tear film distribution is also compromised. For primary lower eyelid surgery for under eye bags, I evaluate the anatomy and function of the lower eyelid using what’s called a pull test, and a snap back test. These tests help me decide if any additional support procedures would be appropriate, such as a lateral tarsal strip to position the lower eyelid for optimal tear distribution. My preferred approach to addressing lower eyelid fat pockets is called a transconjunctival blepharoplasty.
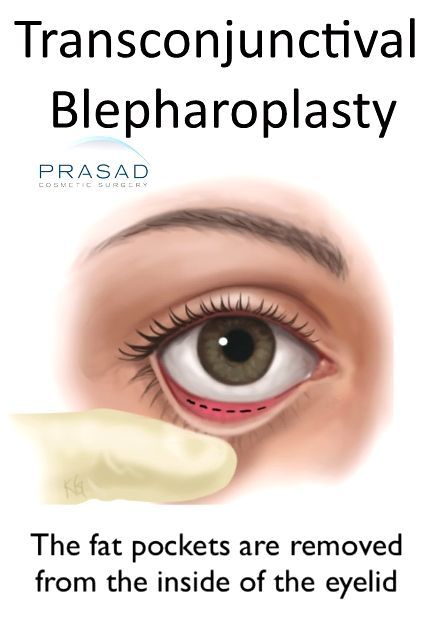
This surgical technique means I address the fat pockets from inside of the eyelid. This technique better preserves lower eyelid support structures, in particular the support muscle called the orbicularis oculi that maintains the position of the eyelid margin for proper tear distribution. I routinely perform this surgery on patients with dry eyes, even those with a history of severe dry eyes.
Additionally, my patients appreciate that there is no visible external scar and the natural shape of the eyes are maintained. Oftentimes people who have dry eyes will actually have improvement in their dry eye symptoms after eyelid surgery. This is because procedures which improve the tone and position of the lower eyelid, combined with the relief of weight from extra skin on the upper eyelid help the eyelids protect and lubricate the eyes. Eyes that look good, function well.
Upper Eyelid Blepharoplasty for Dry Eyes

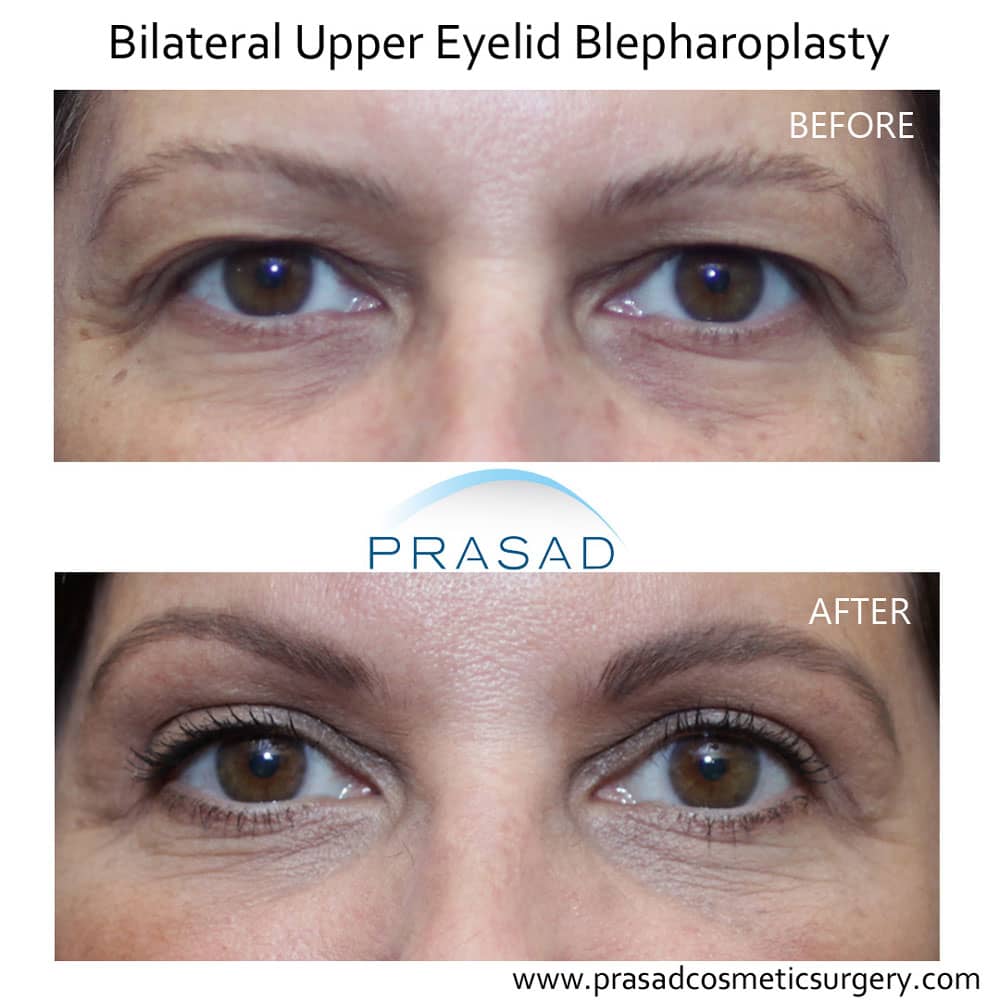
When it comes to upper eyelid surgery, it’s critically important to not remove too much skin, particularly in patients with dry eyes. I would also add that with upper eyelid surgery, particular care must be taken to protect the lacrimal gland, which produces tears. The lacrimal gland exists in the same space where the fat pockets in the upper eyelid are present. When the upper eyelids appear full and heavy, both the fat and the lacrimal gland can be responsible for this appearance. It’s routine to sculpt and remove some fat to create more space, but unfortunately, the lacrimal gland has been mistakenly removed by general plastic surgeons, resulting in a significant loss of tear production.
As an oculoplastic surgeon, during evaluation and during surgery I look for the lacrimal gland, which is often prolapsed or displaced downward. Instead of removing the lacrimal gland, I perform a procedure called lacrimal gland resuspension to restore the anatomical position of the lacrimal gland, and preserve its function.


It’s important to have a clear strategy for dry eye management before, and after surgery. It’s well established that there may be some short-term decrease in tear production after eyelid surgery, so I advise my patients with dry eyes to increase the frequency of using lubricating eye drops prior to surgery. Further, I work with my patients to help them with dry eye management after surgery.
As far as the anesthesia experience, I perform all my eyelid surgeries with local anesthesia with LITE™ IV sedation. My patients recover comfortably and quickly, so they typically return to work in about 1 week.

Can You Have Eyelid Surgery if You Have Dry Eyes?
Yes, cosmetic eyelid surgery can be done safely for people with dry eyes. As mentioned earlier, there are often opportunities to help improve dry eye symptoms with specific procedures, which are well known to oculoplastic surgeons. I would state without reservation that a cosmetic eyelid surgery specialist with training in ophthalmology is ideally suited to perform cosmetic surgery for people with dry eye syndrome.
