Hyaluronic acid fillers, such as those in the Restylane and Juvéderm families, revolutionized how fillers are used in aesthetics in the mid 2000s. Hyaluronic acid fillers are safer, more convenient, and easily metabolized as compared to previous filler materials. Hyaluronic acid is found naturally in the body in places like joint spaces, skin, and even the eye. However, there are some instances where hyaluronic acid filler remains in the body longer than expected. I’ll discuss the reasons why this can happen and how I manage patients with this problem in my practice.
Every day in my practice, I place hyaluronic acid fillers for my patients. With cosmetic fillers, I regularly help people improve the appearance of their lips, under eye hollows, smile lines, and parentheses lines. Thicker hyaluronic acid fillers are also used to restore volume at the bone’s foundational level in areas such as the cheeks, chin (view chin fillers before and after), jaw angle, and jawline. I’m also frequently consulted to reverse hyaluronic acid fillers, and to surgically remove permanent and semi-permanent fillers that were previously placed by other doctors.

Generally, the thickness and viscosity of a hyaluronic acid filler affect its longevity. A thicker filler, such as Juvéderm Voluma, is used in areas where there is less movement, and more projection is required, such as the cheeks. The more viscous Juvederm Voluma can last up to two years. In areas where there is a lot of movement such as the lips and under the eyes, I generally use softer hyaluronic acid fillers such as Restylane-L and Juvederm Volbella. These hyaluronic acid fillers are expected to be metabolized by the body over time.
Can Facial Fillers Go Wrong?
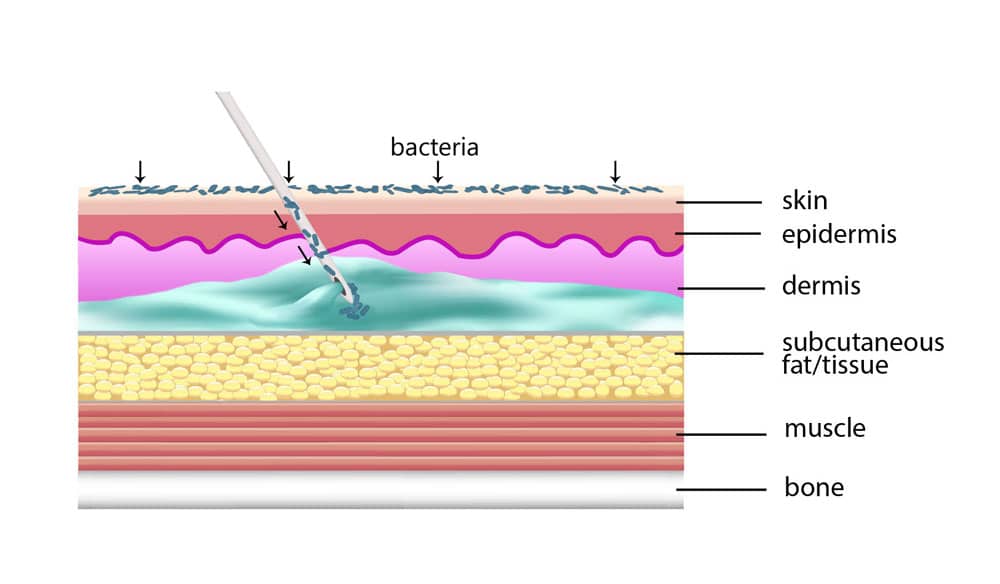
Although hyaluronic acid occurs naturally in the body, there are times when the body reacts by treating the filler as a foreign material. It is unclear whether this reaction is caused by the material itself, or by any surface bacteria that is transferred into the skin during placement.
Nonetheless, the body’s response is to form a capsule around the material. The natural breakdown of hyaluronic acid is prevented when the filler material is surrounded by a capsule. Although this may appear to be a benefit, the appearance is frequently less than ideal. As a result, patients want to find a way to get rid of the hyaluronic acid filler.
What to Do When Facial Fillers Gone Wrong?
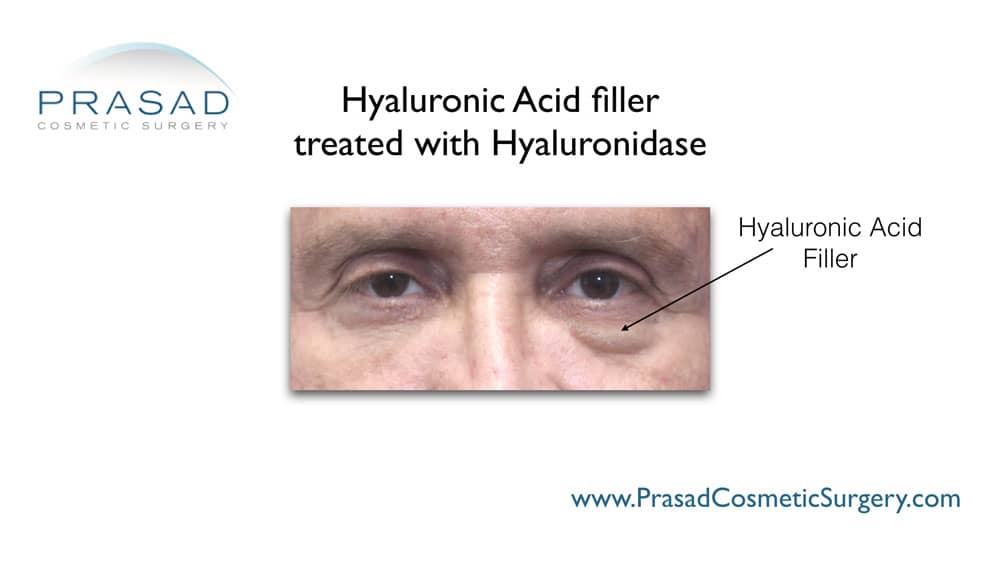
Fortunately, unlike semi-permanent or permanent fillers, encapsulated hyaluronic acid filler treatment involves a strategy to dissolve the filler rather than surgical removal. I use the enzyme called hyaluronidase to dissolve hyaluronic acid. Vitrase and Hylanex are two brand names for hyaluronidase.
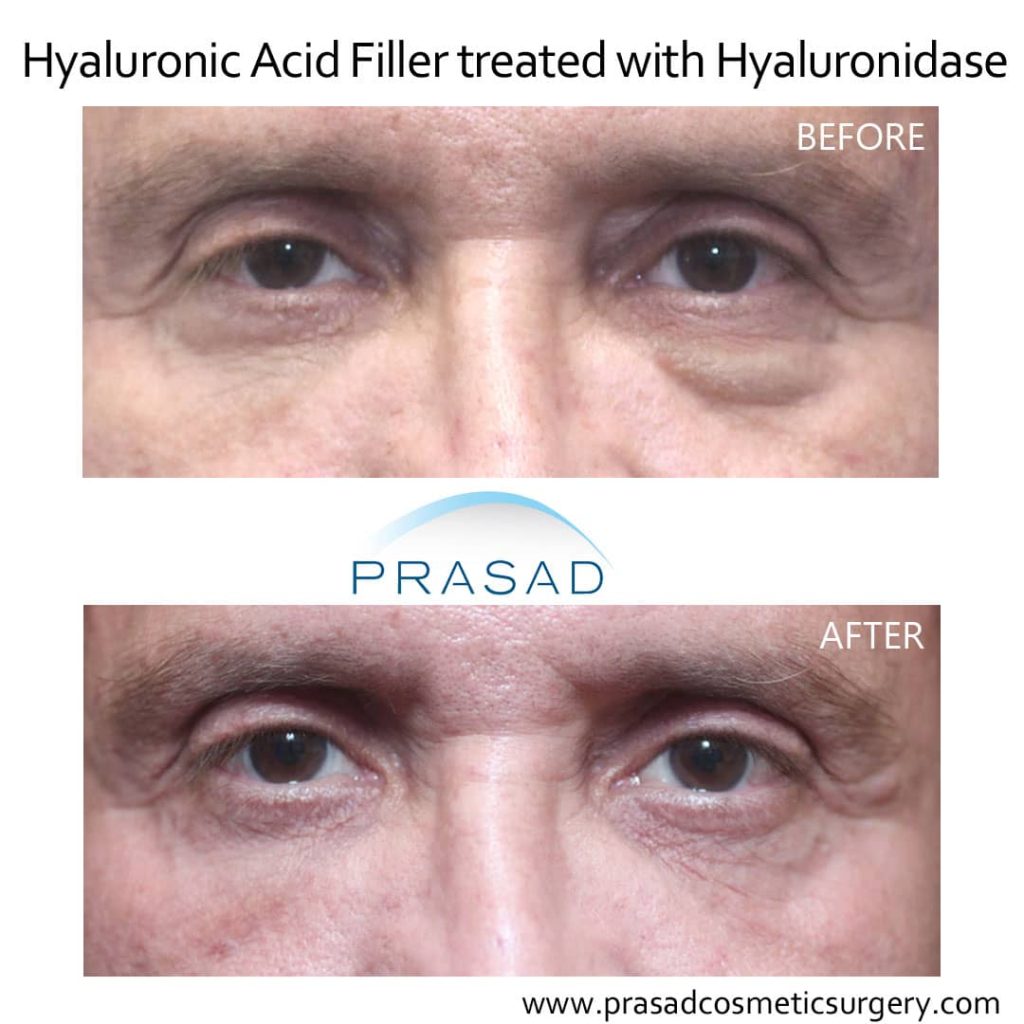


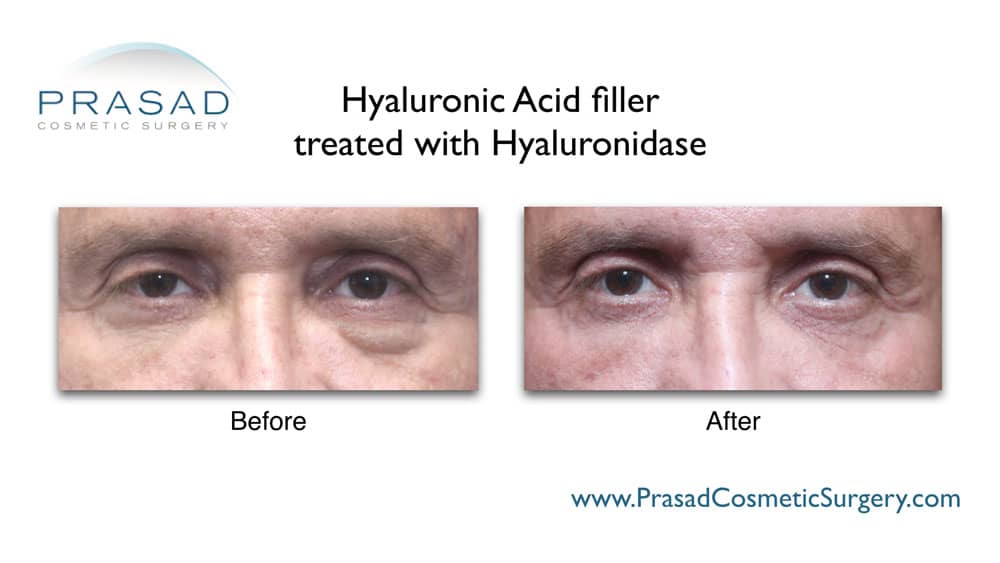
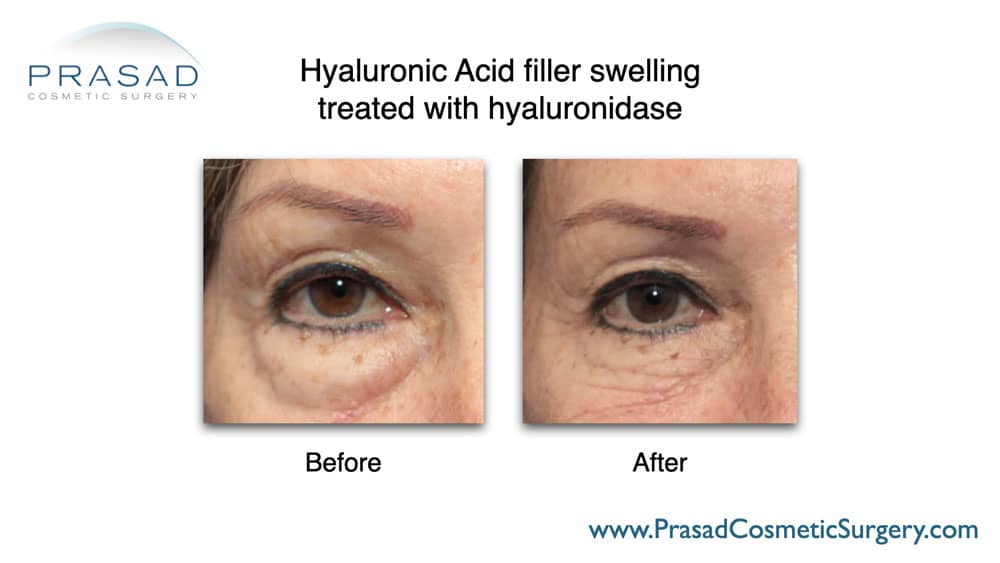

Hyaluronidase is found naturally in your body as part of the normal metabolic processes that produce and metabolize hyaluronic acid. The technical challenge is to be able to place the hyaluronidase inside the encapsulated hyaluronic acid. Once the hyaluronidase contacts the filler material, the material dissolves immediately.
I’ve had several patients who had hyaluronic acid fillers for many years in areas such as the soft tissue of the cheeks, and around the eyes. As I dissolved the filler in the more superficial areas, the patient and I realized that there was more filler in the deeper tissues, which required additional treatment. This simply meant that more sessions would be required until normal anatomy was restored.
Sometimes, patients are surprised to find that the filler they had placed in one area had migrated to an adjacent area. For example, filler placed in the temple to treat hollowing can migrate to the brow, making the brow area appear swollen. A common location where filler migration occurs is the nasolabial fold. Many practitioners try to soften the nasolabial fold by trying to place filler directly under the line. Due to the anatomy of the nasolabial fold, the filler can be displaced upward toward the cheek, and downward toward the lip. Encapsulation of the filler can still occur when the filler has migrated to an area where it was not originally intended.
What is a Biofilm Infection?
As mentioned earlier, bacteria that typically is present naturally on the skin surface can end up on the surface of the injected filler, resulting in an infection called biofilm. In addition to encapsulation, biofilm infection is characterized by periodic episodes of swelling and inflammation. Biofilm is known to occur in different areas of medicine related to any kind of foreign material that is placed past the skin barrier, such as an IV catheter, or a breast implant.
The issue with biofilm is that your immune system is unable to respond to the bacteria effectively due to the absence of blood supply within this foreign material. The standard approach to any infection like this is to remove the foreign material, such as would be the case in the removal of a breast implant. In the case of biofilm associated with hyaluronic acid filler, the strategy is to use hyaluronidase to completely dissolve the hyaluronic acid where the biofilm is residing. The challenge with biofilm infection is often making the diagnosis.
Biofilm is sometimes diagnosed as an immune-mediated problem, in which case the patient is treated with anti-inflammatory medications, in addition to antibiotics. Again, the lack of blood supply makes these strategies difficult and often frustrating. A lot of my patients who come in for hyaluronidase treatment report that they had a hyaluronidase injection performed unsuccessfully by the doctor who had originally performed their filler injection.
I find that many doctors and non-physicians who perform injectables are not as familiar with the tissue anatomy of the areas they’re treating, compared to the level of a surgeon who performs surgery in the same area. Knowledge of the anatomy of the treatment area is particularly relevant around the eyes. Patients are often surprised to learn that an oculofacial plastic surgeon such as myself who trained in the early 90s in ophthalmology, was using hyaluronidase routinely as part of the anesthetic application before cataract surgery. I used hyaluronidase to improve local anesthetic absorption when injecting the local anesthetic behind the eye called a retrobulbar injection.

As an oculoplastic surgeon, I have extensive experience performing surgery around the eye, including the bones and the anatomical spaces around the eye. This means that my knowledge and familiarity in this area are very different from someone who’s never done work like this. Since hyaluronic acid can migrate or be injected into the space deeper than the superficial skin layers, my knowledge and experience in this area have been helpful for people who have had hyaluronic acid injected around their eyes. A common fear is that after hyaluronidase injection, the native natural hyaluronic acid would be dissolved in addition to the filler, potentially resulting in a hollow appearance. In my clinical experience of performing hyaluronidase injections for a wide range of patients for many years, I have not observed any significant issue with hollowing after treatment. Since the body‘s natural hyaluronic acid is continuously replenished, there is no issue in the long-term.
How to Avoid Dermal Filler Complications?
If there is a long-standing hyaluronic acid filler which needs to be removed, the treating physician should have knowledge and experience with both the anatomic spaces, and the precise application of hyaluronidase to achieve the best results.
